Decoding the immune system's defence against Lassa fever in Nigeria

Lassa fever is a viral haemorrhagic fever causing between 100,000 to 300,000 cases and an estimated 5,000 deaths a year in West Africa. In Nigeria, 26% of those diagnosed with Lassa fever die. The disease is caused by Lassa virus (LASV), an RNA virus primarily transmitted by the African rodent, Mastomys natalensis. Transmission occurs through contact with household items and farm grains that have come in contact with the rodent, though to a lesser extent human-to-human transmission (e.g. hospital acquired infection) can occur.
RNA viruses are common causes of emerging diseases because they mutate at a comparatively high rate. There are genetically diverse lineages of the virus found in different parts of West Africa. Symptoms commonly seen in infected people include fever, diarrhoea, weakness, malaise, headache, sore throat, muscle pain, chest pain, nausea, vomiting, diarrhoea, cough, and abdominal pain. There are currently no effective treatments or approved vaccines for Lassa fever.
Based on our work with Lassa patients and survivors in Southern Nigeria from 2018-2020, we have recently published in Nature Scientific Reports (https://rdcu.be/c20qc) our findings of the protective immune response of survivors of Lassa fever, and their exposed contacts. This is key to understanding why some people survive this disease while others do not. The exposed contacts are people who may have provided care to Lassa fever patients, such as family members and clinicians, but have never had a positive diagnosis or clinical symptoms of Lassa fever disease.
A major finding from the study is that the immune responses of both survivors and their exposed contacts make comparable T-cell and binding antibody responses to the Lassa virus. These are critical immune cells and molecular processes that help us fight pathogens. Thus, it was striking to see the similar magnitude of immune responses from both the survivors of the disease who overcame acute symptoms, and their contacts who were never diagnosed nor had any symptoms of the disease. Importantly, one of the distinguishing features between these two groups was that only the survivor’s antibody responses were able to neutralise the virus, while the antibody responses from exposed contacts couldn’t. We hypothesised that this was due to the high levels of virus replication that occur in individuals who develop the disease.
Another important finding from the study is that the virus-neutralising antibody from the survivors were able to eliminate all the genetically diverse lineages of the Lassa virus. Lineage II, which is the dominant Lineage in southern Nigeria, was most effectively neutralized. This is important and promising information for vaccine production because any vaccines targeting one lineage will likely be effective against the other lineages of the virus.
Unfortunately, these T cell and antibody immune responses were found to last less than a decade, suggesting the need for vaccine-boosting in high-risk populations to sustain a protective level of immune responses over time, should vaccination produce a similar immune response to infection. Another finding from our study was that only the survivors retained their binding antibody response for up to 6 months while their exposed contacts didn’t retain these responses at all.
Lastly, we identified the physical components of the virus that induced the strongest T cell responses, suggesting that these regions may serve as strong potential vaccine targets.
In summary, this study is the first description of protective immune responses to Lassa fever in Nigeria. Given that the first generation of Lassa fever vaccines are now entering early-phase clinical trials, this study demonstrated the in-country capacity to perform these assays which will enable further vaccine trials into high-risk populations in affected countries in Africa.
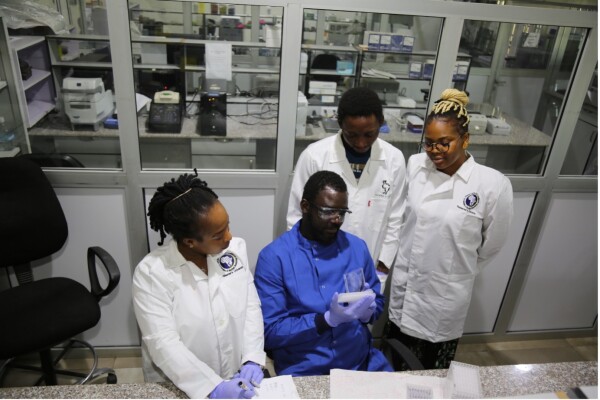
Dr Chinedu Ugwu and the team at ACEGID looking at one of the interferon gamma-specific T cell ELISpot plates
This study was possible because of funding from Project OVEL, granted by the UK’s Biotechnology and Biological Science Research Council (UKRI-BBSRC), as well as by the DFID-Wellcome Epidemic Preparedness grant and support from Cambridge-Africa. It demonstrated the first full transfer of technology and training to Nigeria to establish an in-country capacity to perform immune assays that monitor local immunity to high-consequence infections such as Lassa fever disease in Nigeria. It also paves the way to undertaking vaccine trials in countries where these high-consequence infections are endemic. The knowledge and experiences from this project have now evolved into an immunosurveillance platform called the ARISE platform funded by both the Cambridge-Africa Alborada award and the Bill and Melinda Gates Foundation. The ARISE platform supports pathogen genomic sequencing with real-time, rapid and functional immunologic data that will guide public health response, and vaccine and therapeutics production. Finally, under the supervision of my colleague Dr Storisteanu, Project OVEL has now joined up with UCL researchers to model the impact of climate change on animal-to-human spill-over events of viruses such as Lassa that are major pandemic threats. This project won second prize in the Trinity Challenge last year.
by Dr Ugwu Chinedu, The Africa Centre of Excellence for Genomics of Infectious Diseases (ACEGID), Redeemer's University, Nigeria
Dr Ugwu Chinedu A is a Senior Lecturer and a Postdoctoral Research Fellow at ACEGID, Department of Biological Sciences, Redeemer's University, Ede, Osun State, Nigeria. He is a recipient of a Cambridge-Africa Alborada scholarship.

